| Common Signs & Symptoms | |||||
| Pain | Swelling | Stiffness | Weakness | Instability | Locking |
The Injury
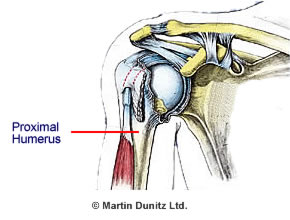
The Humerus is the upper arm bone between the shoulder and the elbow. The part of the Humerus closest to the shoulder is known as the ‘Proximal Humerus’. The Proximal Humerus or upper arm is a common site for a fracture (accounting for around 5% of all fractures). Fractures to the Proximal Humerus generally occur within two distinct groups of people elderly women and adolescents.
A fall onto an outstretched arm is the typical way these fractures occur. In adolescents this is usually caused by high energy trauma (e.g. falling from a tree) while less energy is required to cause a fracture in the older group, because bone strength tends to be diminished by Osteoporosis. Interestingly, what used to be an even distribution between these two groups has changed in recent years in the UK there are now more Proximal Humeral fractures in people aged over 60 who have osteoporosis, than in the adolescent group.
Most Proximal Humerus fractures are uncomplicated, with a stable break that doesn’t need any surgery. However, around 20% of upper arm breaks have complicated fracture lines and displaced fracture fragments which require surgery. An Orthopaedic Consultant will classify the Proximal Humeral fracture depending on the exact location of the fracture lines and fragments.
Signs & Symptoms
There is usually a history of some form of trauma (typically a fall onto an outstretched arm), accompanied by severe pain and an inability to use the affected arm. Suspected Proximal Humeral fractures need to be urgently assessed at the nearest emergency department. To properly assess the extent of the injury the trauma doctor will order x-rays with a front to back view, side view and ‘arm pit’ view. These x-rays from different angles allow the doctor to build up a picture of the fracture lines and fragments. It is important that the fullest picture can be seen because establishing the exact nature of the injury is crucial to getting appropriate treatment. If x-rays can’t provide the full picture, then CT scans may be required.
Treatment
What you can do
| Consult a sports injury expert | |
| Apply a heat pack to relieve pain | |
| Practise exercises to maintain range of movement | |
| Maintain forearm & grip strength with hand therapy exercises | |
| Use resistance bands for shoulder strengthening exercises | |
| Improve balance to help prevent a fall | |
| Use a bone healing system to speed up broken bone healing |
Treatment depends upon the exact fracture pattern, which should be considered together with patient age, general health and the functional demands that will be placed on the arm.
If there is no displacement of the fracture fragments and the fracture is ‘stable’ then conservative treatment is preferable over surgery. The affected arm is immobilised in a Sling for 10-14 days to allow the fracture fragments time to knit together. During this time the patient should practice elbow and wrist movements to prevent these joints becoming stiff. Hand Therapy Balls, Grip Strengtheners and Therapeutic Putty are particularly helpful to maintain forearm and grip strength.
An x-ray is usually repeated two weeks after the injury to check that the fracture fragments are healing in the correct position. If healing is progressing satisfactorily, with the fracture site stable, then physiotherapy treatment can be started to help regain function and limit movement and strength losses.
If there are several fracture fragments it is more likely that the fragments will be displaced. Displaced fragments can heal out of alignment or they may not heal at all (non union). Fracture healing in a non aligned position can lead to Shoulder Impingement Syndrome, so surgery is necessary to restore the normal anatomy. If the fracture pattern shows that there are two or three fragments visible on x-ray then open surgery is appropriate to restore the normal anatomy. The surgeon may use nails, sutures (surgical stitches) or plates and screws to fix the fracture and regain a united bone structure.

If the x-ray shows a fracture pattern with four fragments of the Humerus, or involvement of the shoulder joint surface, then in elderly patients the surgical treatment is usually shoulder ‘hemiarthroplasty’ (pictured below). This is surgical removal of the ball of the shoulder joint known as the Humeral Head, which is replaced with a metal implant. In younger patients the surgeon will usually attempt to restore normal anatomy with surgery. The hemiarthroplasty is very much a last resort in younger people, due to their much better prognosis with rehabilitation.

Following shoulder surgery, Proximal Humeral fractures heal better with physiotherapist supervised rehabilitation. Range of motion exercises are started as early as the surgeon indicates that the fracture is stable, to prevent shoulder stiffness. Many people find that it’s more comfortable to apply a Heat Pack to the shoulder and arm before doing the exercises as there is often residual stiffness from the lack of movement and immobility following a fracture. A Shoulder Support can also provide therapeutic heat.
After six weeks, once the Orthopaedic Consultant is happy that the fracture is healing well, the patient can begin self stretching and pulley exercises to allow the unaffected arm to move the affected arm through its range of movement. More advanced strengthening exercises can begin between six and twelve weeks following the injury. Shoulder strengthening exercises using a Resistance Band are essential.
It is also vital to keep the neighbouring joints as mobile and as strong as possible following a Humeral fracture. The neck in particular can become very stiff due to the prolonged immobility of the shoulder joint. Range of movement exercises and stretches for the neck, elbow and wrist should all be practised to keep the anatomical chain functioning as well as possible and prevent further complications once the fracture has healed.
Prevention
Balance and functional strength training under the supervision of a Chartered Physiotherapist has been shown to be effective in reducing the number of falls in elderly people. Using appropriate walking aids, such as a walking stick or frame or improving in-home safety with handrails has also demonstrated a reduction in the number of falls in older people.


